Recent studies are conducted with view of nutrition in liver disease. Skeletal muscle loss on CT has been associated with accelerated mortality in cirrhotic patients, in overweight cirrhotic patients, in cirrhotic patients awaiting index transplant, and in patients receiving a orthotopic liver transplant.
In a retrospective evaluation of fifty-one pediatric PNALD patients with cirrhosis, the use of a fish-based all-lipid emulsion subsequently changed to a decision of cholestasis in 76% of cases. A randomized controlled study evaluating 100% fish emulsion with soy lipid emulsion each at a dose of 1.0 g /kg/d1 was changed to early termination due to suddenly low prevalence of PNAC. No affected person developed a fatty acid deficiency and each diet was well tolerated and safe.
In randomized controlled trials evaluating SMOF emulsion with whole soybean emulsion, fish containing SMOF emulsion demonstrated that cholestatic liver injury occurs in approximately 50% of people with long-term domestic. In 1985, Bowyer and colleagues defined steatohepatitis in 9 of 60 patients with long-term PN.
There is no published research evaluating the enteral formulation in patients with ALF.In several critically ill patients, it is suggested to avoid the use of any unique formulation in those in a scientific intensive care facility and disorder-specific formulation within the surgical ICU. There is no evidence that the use of BCAA-fortified ENs affects the affected person any better than traditional whole protein formulations in several critically ill patients with liver disorders and are rarely used in the care of ALF patients.
In the control of significantly malnourished ASH patients, a lower survival is expected than for non-malnourished patients.
There is observational research showing nutrition in liver disease and micronutrient deficiencies in people with alcohol and alcoholic liver disorders and very limited research on ASH. Due to poor oral intake preceding extreme illness, micronutrient deficiency should be anticipated and modified in patients with excess ash. Whether or not all patients should be screened for risk of malnutrition or whether or not there should be the usual alternative to micronutrients cannot be answered primarily on the basis of evidence.
Nutrition in chronic liver disease
The diet of people with persistent liver disease is mainly based on a well-known diet with the addition of food supplements if necessary.
Protein malnutrition is a transversal situation at all degrees of continuous liver disease and is found in 65 to 90% of patients with superior impairment.
Retrospective observation has indicated that almost all liver patients are considered for liver transplantation with dietary A and D deficiencies.
Extremely low serum levels of diet D are correlated with improved mortality in patients with ongoing liver problems.
Given the huge consensus that food reputation should be robotically assessed in all people with persistent liver disorders in an effort to understand malnutrition and save you from food exhaustion, improving of a simple, well-confirmed, and reproducible device for dietary reputation assessment in these patients is long overdue. There are no randomized trials evaluating enteral vs parenteral nutrients in patients with HE; however, parenteral nutrients should be considered in excessive cases.Nutritional deficiencies in persistent liver disease are very common and are linked to compromised outcomes in this population.
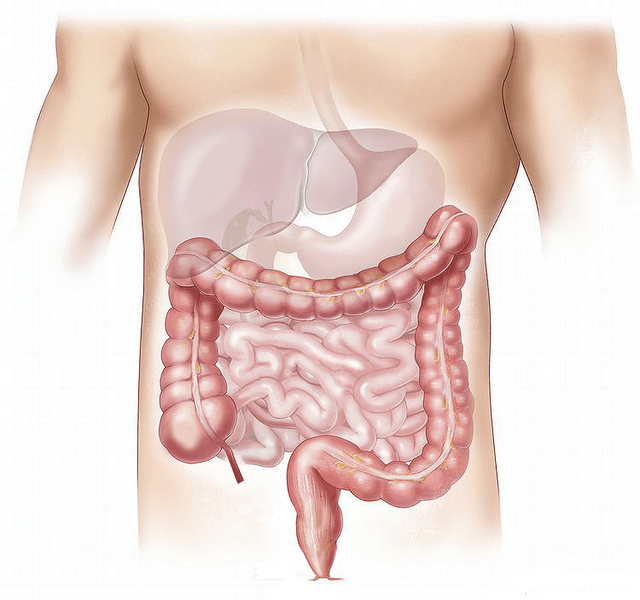
What does the liver do?
The liver has many tasks in the frame. One position is to dump glucose (sugar) for electricity or save it as glycogen. When the liver is not always working properly, your bone structure will depend on several electrical rearrangements made up of proteins (eg muscles) and fatty deposits. You need to avoid letting your muscles down so that you can maintain the power needed to carry out your daily activities.
Preventing Weight Loss
Chronic liver disease, particularly cirrhosis of the liver (upper liver disease) is regularly associated with loss of muscle and structural fat. It may be difficult to see due to fluid gains around the belly or legs.For example, you will lose muscle, but if you train with more fluids, you might gain the same weight.
What am I eating to keep you from losing weight?
To help you save muscle mass and lose fat, you should swallow ingredients with excess power and protein often throughout the day (eg, every 2-3 hours). This is vital for humans with persistent liver disorders, as protein is used to maintain muscle tissue and frame tissue (such as the liver) and to maintain normal frame function.
Nutrition in liver disease recommendations for clinical practice Measures of frailty, defined as the patient’s vulnerability to stress, reduced physiological reserve and lack of practical popularity.
Several pharmacological treatments have been proposed to increase bone mass in patients with persistent liver disease, but most research has protected a small number of patients, and therefore it is difficult to draw firm conclusions.