Uses of beets (Beta vulgaris) and molasses (Saccharum officinarum)
June 12, 2022
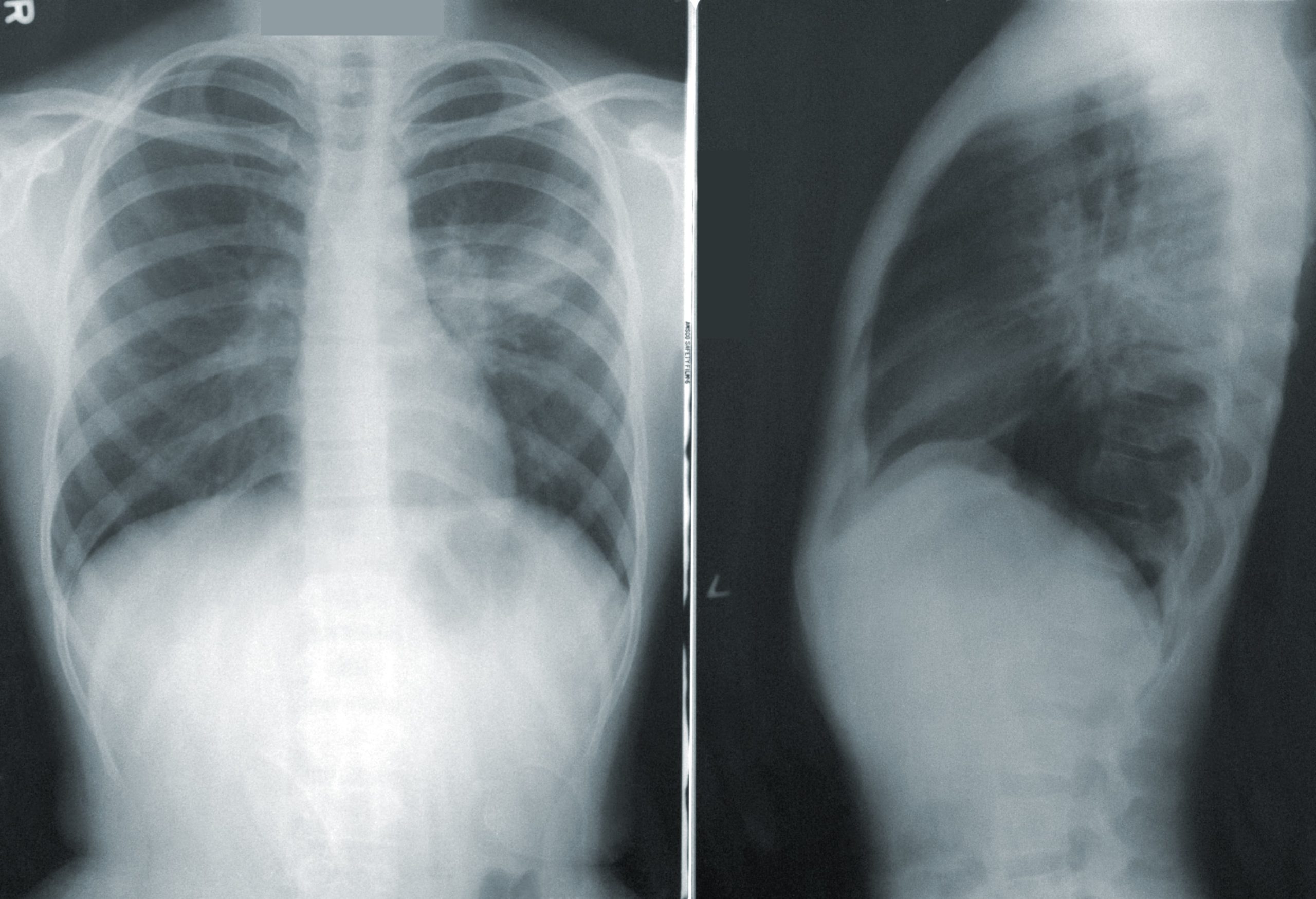
Pneumonia is the 6th main reason for loss of life in the United States and the primary reason for loss of life from infectious diseases. The patients are treated in the Intensive care unit (ICU) using various means of the treatment course.
Pneumonia is not uncommon among clinical ailments because its pathogenesis, remedy, and prevention may be discussed, however, there’s a lot of controversy about the correct way of its management.
THERAPY
If diagnostic checking out famous a selected etiologic pathogen, a remedy may be centered on the results. In addition, as referred to earlier, if an expected pathogen isn’t found in a diagnostic sample, it could be feasible to prevent empiric insurance of that organism.
General Considerations
Until recently, a mixture of empirical antibiotic remedies for intense pneumonia was universally used using physicians running in ICUs. However, most effective with bacteria P. aeruginosa pneumonia (commonly with an aminoglycoside and a β-lactam) has been proven to be advanced to monotherapy. One disadvantage is the aminoglycosides themselves, a category of antibiotics with a slender therapeutic-to-poisonous ratio, and an excessive prevalence of nephrotoxicity.
This method is theoretically feasible due to the extended post-antibiotic impact of aminoglycosides, and it’s far been hoped that once-day-by-day dosing can enhance efficacy, reduce (or as a minimum now no longer increase) toxicity, and decrease the want for tracking of serum levels.
Antipseudomonal β-lactam antibiotics encompass the penicillins( piperacillin, azlocillin, mezlocillin, ticarcillin, and carbenicillin;) the third-generation cephalosporins ceftazidime and cefoperazone; the fourth-era cephalosporin cefepime; the carbapenems imipenem and meropenem; the monobactam aztreonam (which may be used within the penicillin-allergic affected person); and the β-lactam/β-lactamase inhibitor combos ticarcillin/clavulanate and piperacillin/tazobactam. Other antipseudomonal retailers encompass the quinolone ciprofloxacin; excessive-dose levofloxacin; and the aminoglycosides (amikacin, gentamicin, tobramycin).
Community-Acquired Pneumonia (CAP)
For ICU-admitted community-acquired pneumonia, preliminary remedies need to be directed at DRSP, Legionella and different pathogens, enteric gram-negative, and different decided on organisms on the premise of epidemiologic assessment. In all, no ICU-admitted community-acquired pneumonia affected person needs to obtain empirical monotherapy, despite one of the new quinolones.
This advice is primarily based on the reality that the efficacy (in particular for meningitis complicating pneumonia), powerful dosing, and protection of quinolone monotherapy have now no longer been set up for ICU-admitted CAP sufferers. Information on the right therapy for CAP patients is scarce. Even within the presence of pneumococcal bacteremia, quick periods of therapy can be feasible, with transfer from intravenous to oral remedy in responding patients.
Nosocomial Pneumonia
Antibiotic therapy is given to primary medical suspicion of pneumonia. Empirical remedies need to be dictated only when the affected person is a threat of contamination with MDR pathogens, commonly due to the presence of new antibiotic remedies, an extended health center stays.
If the affected person is allergic to penicillin, the remedy may be with a quinolone or a mixture of clindamycin and aztreonam.
Conclusion
Therefore it’s far vital to screen resistance and to pick out an empirical therapy. One different idea that has been integrated into a few research on empirical remedies is that of “antibiotic rotation,” i.e. the same old empirical regimens are deliberately numerous over the years to show microorganisms to specific antibiotics and for that reason limit the choice strain for resistance.
Combination therapy is maximally preferred as it is broad-spectrum, thereby minimizing the risk of, beginning with, irrelevant treatment regimens. Aerosolized management of antibiotics gives the gain of attaining excessive concentrations of antibiotics. Locally administered antibiotics are hardly ever absorbed, and systemic toxicity is minimized. Despite those theoretical advantages, many efficacy questions continue to be spoken back with the aid of using medical trials.